First Author: Monica Verdoia
Division of Cardiology, Azienda Ospedaliera-Universitaria “Maggiore della Carità”, Eastern Piedmont University, Novara, Italy.

Commentary on: Vitamin D deficiency is independently associated with the extent of coronary artery disease
By Ilaria Coccia, Policlinico Tor Vergata, Roma
Vitamin D is a secosteroid hormone, well known for its role in calcium and phosphate metabolism and bone health homeostasis. In the last decades, a stronger evidence about the correlation between vitamin D and coronary artery disease (CAD) is spreading in the Scientific Community. This is the first large study to investigate the relationship between vitamin D levels and the extent of CAD.
Some studies showed that the binding of vitamin D to vitamin D receptor (VDR) regulates numerous genes involved in cell proliferation and differentiation, apoptosis, oxidative stress, membrane transport, matrix homeostasis and cell adhesion. Merke et al. demonstrated the presence of VDR in bovine aortic endothelial cells and in human dermal capillaries and Norman and J.T. Powell discovered a real vitamin D micro-endocrine system in the cardiovascular cells.
These discoveries opened the way to further studies about the connection between Vitamin D levels and myocardial infarction. Vitamin D may modulate the pathogenesis of atherosclerosis influencing the immune system: on the one hand it increases the expression of anti-inflammatory cytokines such as IL-10 and on the other hand it decreases the expression of pro-inflammatory molecules, it suppresses TH1 and TH17 cells favouring the differentiation of Treg and TH2 cells.[59] Both 1,25(OH2) D and 25(OH)D inhibit the production of tumour-necrosis factor-α (TNFα) and IL- 6 by targeting monocyte/macrophage mitogen-activated protein kinase phosphatase-1. This is highly relevant to atherosclerosis given that cytotoxic T cells and leukocytes’ enzymes, as matrix metalloproteinase 9 (MMP-9), promote the vulnerability of the plaque.
Vitamin D also plays a role in vascular calcification, a multifactorial process with deep clinical implications. In addition to this everal papers have reported a relationship between vitamin D levels and Hypertension, describing Vitamin D as a negative regulator of the renin-angiotensin-aldosterone system (RAAS) in VDR knockout models.
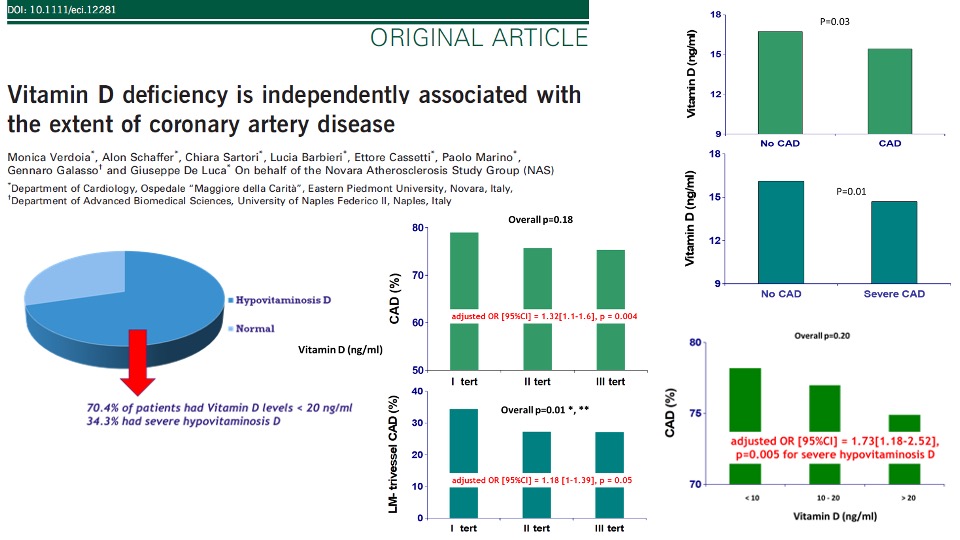
Verdoia et al. enrolled 1484 patients undergoing elective angiography in a cross-sectional study. Hypovitaminosis D was observed in 70.4 % of them. Patients were divided into vitamin D tertiles (<9.6;9.6-18.4;18.4) and after a data adjustment for baseline characteristics (age, gender, renal failure, smoking, acute presentation, calcium antagonists, diuretics, beta-blockers, statins, haemoglobin, platelet count, total and LDL cholesterol, triglycerides), the association between vitamin D levels and CAD reached a statistical significance (adjusted OR [95%CI] = 1.32[1.1–1.6], P = 0004). Moreover, vitamin D levels were significantly lower in patients with severe CAD (adjusted OR[95% CI] = 1.73[1.18–2.52], P = 0005), and especially for patients with vitamin D values < 10 ng/mL, that should be regarded as those at higher potential cardiovascular risk. In addition, Verdoia et al. identified a significant association between vitamin D and major risk factors, finding that vitamin D is directly related to haemoglobin levels (P < 0001) and inversely to platelet count (P = 0002), total and low-density-lipoprotein (LDL) cholesterol (P = 0002 and P < 0001, respectively) and triglycerides (P = 001).
However, despite this clinical evidence, contrasting results have been reported with cholecalciferol supplementation in cardiovascular prevention and further studis are nedeed to establish if vitamin D could be used in the prevention and therapy of CAD.
Read more: https://pubmed.ncbi.nlm.nih.gov/29656938/
