Authors:
Enrico Guido Spinoni 1-2, Marco Mennuni 2, Andrea Rognoni 2, Leonardo Grisafi 1-2, Crizia Colombo 1-2, Veronica Lio 1-2, Giulia Renda 3, Melissa Foglietta 3, Ivan Petrilli 3, Damiano D’Ardes 3, Pier Paolo Sainaghi 1-2, Gianluca Aimaretti 1-2, Mattia Bellan 1-2, Luigi Castello 1-2, Gian Carlo Avanzi 1-2, Francesco Della Corte 1-2, Marco Krengli 1-2, Mario Pirisi 1-2, Mario Malerba 1-4, Andrea Capponi 2, Sabina Gallina 3, Sante Donato Pierdomenico 3, Francesco Cipollone 3, Giuseppe Patti 1-2, COVID-UPO Clinical Team.
Affiliations:
1 Università del Piemonte Orientale, Novara; 2 AOU Maggiore della Carità, Novara; 3 Università Gabriele d’Annunzio, Chieti-Pescara; 4 Ospedale Sant’Andrea, Vercelli.
Commentary
Atrial fibrillation (AF) shares with CoronaVirus Infective Disease (COVID-19) various prevalent cardiovascular (CV) co-morbidities (1-2). The occurrence of AF in patients with COVID-19 and its impact on outcome have not been specifically evaluated yet.
We investigated the incidence and prognostic impact of different subgroups of AF (historical and new onset) in consecutive patients hospitalized for COVID-19. A total of 637 patients, admitted in three major Italian hospitals, were included. In-hospital outcomes were investigated, choosing as primary endpoint the incidence of all-cause mortality and as secondary endpoints: the occurrence of CV death, non-CV death and severe acute respiratory distress syndrome (ARDS).
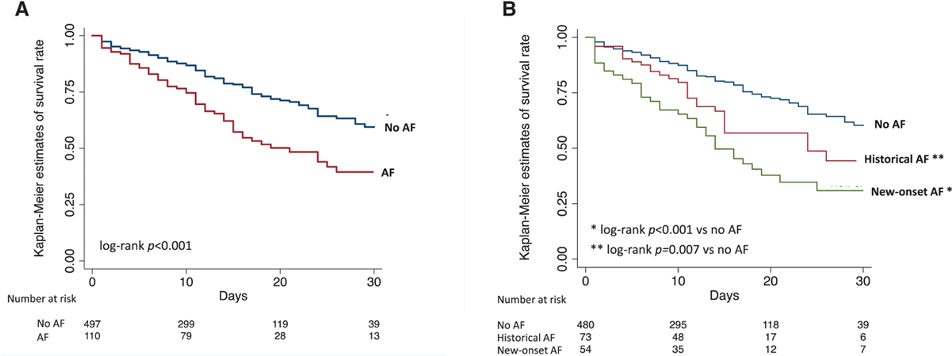
We included a total of 637 patients, 503 (79%) patients with stable sinus rhythm, and 134 (21%) in-hospital AF (historical in 79 patients and new-onset in 55). Patients with AF were older and presented a higher prevalence of various comorbidities: arterial hypertension, diabetes, cardiomyopathy, peripheral artery disease, chronic kidney disease, and chronic obstructive pulmonary disease. Our study outlined higher in-hospital mortality in patients with AF (44.4% versus 22.1% in those without, P=0.001); 30-day estimated survival rates by Kaplan-Meier method were 39.6% (95% CI, 27.8%–50.8%) versus 59.4% (51.4%–66.5%), respectively (log-rank P<0.001; Figure panel A). We performed logistic regression analysis, including demographic
factors, comorbidities, laboratory findings, and in-hospital treatments. At multivariate analysis the occurrence of AF was significantly associated with an increased risk of all-cause death (OR 2.44, 95% CI 1.18-5.07; p=0.016), CV death (OR 3.26, 95% CI 1.2–9.5; p=0.03) and severe ARDS (OR 1.96, CI 95% 1.07-3.6; p=0.03).
Patients with new-onset AF showed an increased incidence of in-hospital death (49.1% versus 36.7%), cardiovascular mortality (14.6% versus 5.1%), and ARDS (49.1% versus 29.7%)
compared with those with historical AF. The 30-day estimated survival rates were 44.3% (95% CI, 27.7%–59.6%) in patients with historical AF (log-rank p=0.007 versus no AF) and 30.8% (17.4%–45.2%) in those with new-onset AF (log-rank p<0.001 versus no AF; Figure [B]). Using patients without AF as reference, a stepwise increase in the risk of all-cause death across patients with historical AF (adjusted OR 1.26, 0.58-2.74) and those with new onset AF (adjusted OR 3.34, 1.54-7.25) was demonstrated.
Our study suggests the hypothesis that new-onset of AF in patients hospitalized for COVID-19 represent an independent predictor oin-hospital mortality, CV death, and more severe clinical pattern. In such setting, new-onset AF may represent potential clinical marker of adverse outcomes, as it is associated by higher degree of inflammatory and hypoxemic viral insult.
In conclusion, our study support the hypothesis that in patients hospitalized for COVID-19, the occurrence of AF is frequent and is independently associated with adverse outcome, including increased all-cause and cardiovascular mortality.
Figure: Kaplan-Meier curves at 30 days. Estimates of survival stratified by presence/absence of atrial fibrillation (AF; A) and by AF subtypes (B) are illustrated.
References:
1. Palmieri L, Vanacore N, Donfrancesco C, Lo Noce C, Canevelli M, Punzo O, Raparelli V, Pezzotti P, Riccardo F, Bella A, et al.; Italian National Institute of Health COVID-19 Mortality Group. Clinical characteristics of hospitalized individuals dying with COVID-19 by age group in Italy.J Gerontol A Biol Sci Med Sci. 2020; 75:1796–1800.
2. Inciardi RM, Adamo M, Lupi L, Cani DS, Di Pasquale M, Tomasoni D, Italia L, Zaccone G, Tedino C, Fabbricatore D, et al. Characteristics and outcomes of patients hospitalized for COVID-19 and cardiac disease in Northern Italy.Eur Heart J. 2020; 41:1821–1829.
Read more on:
Figura